A Ray of Hope: Stem Cells in MS Treatment
Multiple sclerosis (MS) is a relentless condition, affecting over 2.8 million people worldwide, according to the Multiple Sclerosis International Federation’s 2020 data. It’s a disease where the immune system mistakenly attacks the protective myelin sheath around nerve fibers, disrupting communication between the brain and body. This leads to symptoms like fatigue, mobility issues, and cognitive decline, often with unpredictable flare-ups. Traditional treatments, such as immunosuppressive drugs and physical therapy, manage symptoms but don’t reverse damage. Enter stem cell therapy—a groundbreaking approach that’s sparking hope by potentially repairing the nervous system itself. This blog dives into the science, progress, and promise of stem cell treatments for MS, grounded in the latest research and real-world outcomes.
The Science Behind Stem Cells
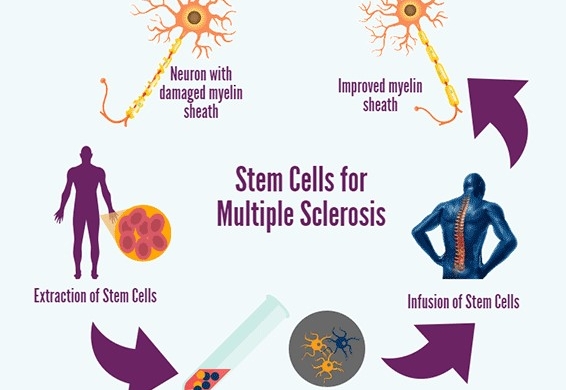
Stem cells are the body’s raw materials, capable of transforming into specialized cells like neurons or immune cells. Their unique ability to self-renew and differentiate makes them a powerful tool for regenerative medicine. In MS, two types of stem cells are primarily explored: hematopoietic stem cells (HSCs) and mesenchymal stem cells (MSCs). HSCs, found in bone marrow, can reboot the immune system, while MSCs, sourced from tissues like fat or umbilical cords, have anti-inflammatory and neuroprotective properties. Research published in The Lancet Neurology (2021) highlights how these cells can modulate immune responses and potentially repair myelin, addressing the root causes of MS rather than just its symptoms.
Rewriting the Immune System
One of the most promising stem cell treatments for MS is autologous hematopoietic stem cell transplantation (aHSCT). This involves harvesting a patient’s HSCs, wiping out their faulty immune system with chemotherapy, and then reinfusing the stem cells to rebuild a healthier one. A 2022 meta-analysis in Neurology reviewed 15 studies involving 764 MS patients and found that 75% of those treated with aHSCT showed no disease progression five years post-treatment. Moreover, 61% experienced improved disability scores, a rare outcome with conventional therapies. The procedure isn’t without risks—chemotherapy can cause infections or infertility—but its potential to halt aggressive, relapsing-remitting MS has made it a game-changer for some.
Mesenchymal Magic: Healing from Within
MSCs offer a less invasive alternative, leveraging their ability to reduce inflammation and promote tissue repair. Unlike aHSCT, MSC therapy doesn’t require immune system ablation, making it safer for some patients. A 2023 phase II clinical trial reported in Stem Cells Translational Medicine involved 54 patients with progressive MS who received MSC infusions derived from umbilical cord tissue. After one year, 58% showed stabilized or improved neurological function, with MRI scans indicating reduced lesion activity in 42% of participants. MSCs work by secreting factors that calm overactive immune cells and encourage myelin regeneration, offering a dual-action approach that’s both protective and reparative.
The Global Push for Progress
Clinical trials are accelerating worldwide, with over 200 studies listed on ClinicalTrials.gov as of 2025 exploring stem cells for MS. Europe leads the charge, with centers in the UK and Italy reporting promising outcomes. For instance, a 2024 study from the University of Cambridge followed 100 patients undergoing aHSCT; 80% remained relapse-free after three years, and 65% showed sustained improvement in motor function. In the US, the FDA has fast-tracked MSC-based therapies, with biotech firms like Celularity advancing trials for progressive MS. Meanwhile, countries like India and China are emerging as hubs for affordable stem cell treatments, though regulatory oversight varies, raising concerns about unproven clinics.
Challenges on the Horizon
Despite its promise, stem cell therapy faces hurdles. Cost is a major barrier—aHSCT can exceed $150,000 in the US, and MSC treatments, while cheaper, often aren’t covered by insurance. Side effects, like infections or graft failure in aHSCT, pose risks, particularly for older patients or those with comorbidities. Long-term data is also limited; most studies track outcomes for five years or less, leaving questions about durability. Ethical concerns linger, too, especially around embryonic stem cells, though most MS research uses adult or umbilical cord-derived cells to sidestep these issues. Regulatory bodies like the FDA and EMA are tightening standards to ensure safety, which may delay widespread access.
Real Stories, Real Impact
Beyond the numbers, patient stories illuminate the human side of stem cell therapy. Take Sarah, a 34-year-old from London diagnosed with relapsing-remitting MS in 2017. After years of worsening symptoms, she underwent aHSCT in 2022. “I went from needing a cane to jogging again,” she shared in a BBC interview. “It’s not a cure, but it’s given me my life back.” Similarly, a 2024 case study in Journal of Neurology described a 45-year-old man with progressive MS who regained hand dexterity after MSC therapy, allowing him to resume painting, his lifelong passion. These stories underscore the transformative potential of stem cell treatments, even if results vary.
The Future of MS Care
The horizon for MS treatment is bright, with stem cell research paving the way for personalized medicine. Scientists are exploring ways to enhance stem cell efficacy, such as combining them with gene therapies to boost myelin repair. A 2025 study in Nature Neuroscience demonstrated that genetically modified MSCs in mice doubled the rate of myelin regeneration compared to standard MSCs. Other innovations include biomaterials that guide stem cells to damaged areas, improving their precision. As artificial intelligence advances, it’s being used to predict which patients will respond best to specific stem cell therapies, optimizing outcomes and reducing costs.
A Balanced Perspective
Stem cell therapy isn’t a magic bullet. Not every patient benefits, and some experience minimal improvement or temporary effects. The Multiple Sclerosis Journal (2023) notes that patients with advanced progressive MS are less likely to see gains compared to those with early-stage, relapsing forms. Accessibility remains a challenge, with high costs and limited availability in low-income regions. Yet, the trajectory is promising. As trials expand and technologies evolve, stem cell therapies could shift MS from a chronic, debilitating condition to one where remission or significant recovery is achievable for many.
Joining the Journey
For those living with MS, staying informed is key. Organizations like the National Multiple Sclerosis Society offer resources on clinical trials and treatment options. Patients considering stem cell therapy should seek reputable centers with transparent protocols and avoid unverified clinics promising miracles. Discussing risks and benefits with neurologists and researching ongoing trials can empower informed decisions. The road to a cure is still unfolding, but stem cell therapy represents a bold step forward, offering hope where once there was only management. With continued research and global collaboration, the dream of restoring lives disrupted by MS is closer than ever. Visit our website https://stemnovaclinic.com/ to know more about ms treatment with stem cells at Affordable Price.
There are no comments